Types Of Cancer We Treat
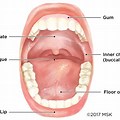
Oral Cavity Cancer
All you need to know
A lesser-known but extremely serious health issue, oral cancer impacts millions of individuals globally. One kind of cancer that begins in the mouth is oral cancer, sometimes known as mouth cancer. Lips, tongue, gums, cheeks, the floor of the mouth, and even the tonsils are among the areas of the mouth that may be impacted. Even though they are frequently overlooked, these malignancies can be fatal if ignored or mistreated.
Causes and Risk Factors
Tobacco and Alcohol Use: Among the most significant risk factors for oral cancer are tobacco products in various forms, including smoking and smokeless tobacco, as well as excessive alcohol consumption. The combined use of tobacco and alcohol substantially elevates the risk of developing this type of cancer. Human Papillomavirus (HPV): Certain strains of HPV have been linked to oral cancer, making HPV infection a notable risk factor. This is especially pertinent for younger individuals. Sun Exposure: Prolonged exposure to sunlight, particularly on the lips, can increase the risk of developing lip cancer. Protection from the sun’s harmful UV rays is advisable. Dietary Habits: A diet low in fruits and vegetables may be a risk factor for oral cancer. Conversely, a diet rich in these foods is associated with a lower risk.Clinical Symptoms
Timely recognition of the warning signs and symptoms of oral cancer is pivotal. If you experience any of the following, it is strongly advisable to seek immediate consultation with a healthcare professional: Persistent Oral Sores: The presence of persistent mouth sores that do not heal as expected. Lesions: Red or white patches appearing in the oral cavity. Hoarseness or Sore Throat: Persistent sore throat or hoarseness without any discernible cause. Difficulty in Swallowing or Chewing: Impairment in the ability to swallow or chew. Unexplained Swellings: The development of swelling, lumps, or abnormal bumps in the mouth, neck, or throat. Numbness or Pain: Experiencing unexplained numbness or pain in the lips, tongue, or other regions of the oral cavity. Unexplained Weight Loss: Significant, unintended weight loss that lacks a clear underlying reason.Treatment & Rehabilitation of oral cancer
It varies depending on the stage of the disease, the location and size of the tumor, and the overall health of the patient. Here are the main approaches to treating oral cancer: Surgery Intervention: Surgical removal of the tumor is a common treatment for oral cancer. This may involve removing the tumor itself or excising affected tissues, such as lymph nodes in the neck. In cases where extensive surgery is necessary, reconstructive surgery may be performed to restore function and appearance. Radiation Therapy: Radiation therapy employs high-energy X-rays or other radiation sources to target and destroy cancer cells. It can be used as the primary treatment for smaller tumors or as adjuvant therapy after surgery to eliminate any remaining cancer cells. Chemotherapy: Chemotherapy uses drugs to either kill cancer cells or inhibit their growth. It is often used in conjunction with radiation therapy, especially for advanced-stage oral cancers or when the cancer has metastasized to other parts of the body. Targeted Therapy: In some cases, oral cancers with specific molecular characteristics may be treated with targeted therapies. These drugs are designed to disrupt the specific pathways contributing to cancer growth. Immunotherapy: Immunotherapy is an emerging treatment that works by stimulating the patient’s immune system to recognize and combat cancer cells. While it’s not yet a standard treatment for all oral cancers, ongoing research is exploring its potential. Palliative Care: For advanced oral cancer that is challenging to treat or when treatment is no longer effective, palliative care becomes essential. It focuses on symptom management, improving the patient’s quality of life, and providing emotional support. Rehabilitation: After treatment, patients may require rehabilitation to regain normal function, particularly when surgery impacts their ability to eat, speak, or swallow. Speech therapy, physical therapy, and dietary adjustments may be part of the rehabilitation process. Follow-Up Care: Regular follow-up appointments are essential to monitor for recurrence or complications. Early detection of potential issues can lead to more effective intervention. The choice of treatment depends on the specific case and the patient’s overall health. Treatment decisions should be made following a comprehensive evaluation and discussion with a healthcare team. In many cases, a combination of treatment modalities is used to maximize effectiveness and reduce the risk of recurrence. Early detection and timely treatment significantly improve the chances of successful outcomes for oral cancer patientsPreventive Strategies
Preventing oral cancer primarily hinges on informed lifestyle choices and early detection methods: Tobacco and Alcohol Abstinence: The most effective risk-reduction strategy for oral cancer is complete cessation of tobacco use, encompassing smoking and smokeless forms, along with moderating alcohol intake. HPV Vaccination: The vaccination against high-risk HPV strains is pivotal in reducing the likelihood of HPV-related oral cancers. Sun Protection: Employ lip balm with a sun protection factor (SPF) and exercise prudence in sun exposure to safeguard the lips from harmful ultraviolet (UV) rays. Nutrient-Rich Diet: Embrace a balanced diet teeming with fruits and vegetables, as they offer indispensable nutrients and antioxidants that may aid in cancer prevention. Regular Dental Check-ups: Consistently scheduled dental visits provide a channel for oral screenings, enabling the early detection of oral cancer during routine examinations.Laryngeal cancer

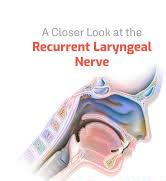
Throat cancer refers cancer that develops in your throat (pharynx) or voice box (larynx). Throat cancer is a general term that applies to cancer that develops in the throat (pharyngeal cancer) or in the voice box (laryngeal cancer). Signs and symptoms of throat cancer may include: A cough Changes in your voice, such as hoarseness or not speaking clearly Difficulty swallowing Ear pain A lump or sore that doesn’t heal A sore throat Your treatment options are based on many factors, such as the location and stage of your throat cancer, the type of cells involved, whether the cells show signs of HPV infection, your overall health, and your personal preferences. Discuss the benefits and risks of each of your options with your doctor.
Thyroid & Parathyroid cancers
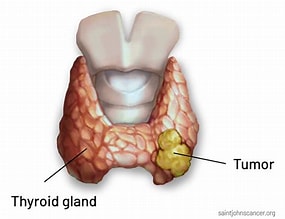
Thyroid cancer is a malignant condition that originates in the thyroid gland situated in the neck. This cancer emerges when thyroid cells undergo abnormal growth, resulting in the formation of tumors. Although relatively uncommon, it ranks among the most prevalent cancers affecting the endocrine system. Thyroid cancer is typically treatable, particularly when diagnosed at an early stage. It may manifest with symptoms such as a painless neck lump, voice changes, or difficulty swallowing. Diagnosis involves physical examinations, medical imaging (e.g., ultrasound), and biopsies. Treatment options, including surgery, radioactive iodine therapy, and thyroid hormone replacement, are contingent upon the type and stage of the cancer. Timely diagnosis and suitable treatment are critical for achieving better outcomes. Symptoms: Lump or Nodule: The most frequent indication of thyroid cancer is the presence of a painless lump or nodule in the neck. These lumps may sometimes be self-detected or uncovered during routine medical check-ups. Neck Swelling: As the thyroid cancer tumor grows, it can lead to noticeable swelling in the neck, often more prominent on one side. Neck or Ear Pain: Some individuals with thyroid cancer experience neck or ear discomfort, though this symptom may not be present in all cases. Voice Changes: Thyroid cancer can impact the vocal cords, resulting in hoarseness or changes in one’s voice. Persistent voice changes, especially in non-smokers, warrant investigation. Difficulty Swallowing: Large thyroid tumors can obstruct the swallowing process, causing discomfort and a sensation of a lump in the throat. Coughing or Breathing Problems: In rare instances, thyroid cancer may extend into the airway, causing coughing or breathing difficulties, which is more commonly associated with the highly aggressive anaplastic thyroid cancer. Diagnosis: Physical Examination: Healthcare providers examine the thyroid gland for nodules or irregularities during a physical examination. If a nodule is detected, further evaluation is necessary. Imaging Tests: Detailed images of the thyroid gland are obtained through ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI) scans, aiding in assessing nodule or tumor characteristics. Fine-Needle Aspiration (FNA) Biopsy: FNA biopsy involves using a thin needle to collect a tissue sample from a thyroid nodule. This sample is examined under a microscope to identify cancer cells. Blood Tests: While not a direct diagnostic method for thyroid cancer, blood tests measure thyroid hormone levels, providing insight into overall thyroid function. Risk Factors: Gender: Thyroid cancer is more prevalent in women than in men, with women being three times more likely to develop the disease. Age: The risk of thyroid cancer increases with age, with the highest incidence occurring in individuals between 30 and 60 years old. Family History: A family history of thyroid cancer, particularly in first-degree relatives (parents, siblings), increases the risk. Radiation Exposure: Exposure to ionizing radiation, especially during childhood, is a significant risk factor. This includes radiation therapy for head and neck cancers and radiation exposure from nuclear accidents. Dietary Iodine: Diets with either insufficient or excessive iodine intake may be associated with an increased risk of thyroid cancer, emphasizing the importance of balanced iodine intake. Types: Papillary Thyroid Cancer: Accounting for approximately 80% of all cases, this type is typically slow-growing and highly treatable. Follicular Thyroid Cancer: Representing 10-15% of thyroid cancers, it tends to stay confined within the thyroid but can be more aggressive than papillary cancer. Medullary Thyroid Cancer: Originating in parafollicular cells or C cells, this cancer accounts for about 4% of thyroid cancers and can spread to lymph nodes and other areas. Anaplastic Thyroid Cancer: This rare and extremely aggressive form does not respond well to treatment. Thyroid Lymphoma: Affecting the lymphatic system within the thyroid, this is a rare subtype of thyroid cancer. Staging of Thyroid Cancer: Thyroid cancer is typically staged using the American Joint Committee on Cancer (AJCC) TNM system, which considers the tumor (T), lymph nodes (N), and distant metastasis (M). Stage 0: Cancer is confined to the thyroid without invasion or spread. Stage I: The tumor is small and limited to the thyroid. Stage II: The tumor is larger but still contained within the thyroid. Stage III: Cancer may be any size but has extended beyond the thyroid. Stage IVA: Cancer has spread to nearby lymph nodes. Stage IVB: Cancer has spread to lymph nodes in the upper chest. Stage IVC: Cancer has spread to distant sites or organs (metastasis). Staging guides treatment decisions and provides insight into prognosis. Treatment: Surgery (Thyroidectomy): The primary treatment typically involves surgically removing the thyroid gland or the affected portion. Radioactive Iodine (RAI) Therapy: After surgery, RAI therapy may be used to eliminate remaining cancer cells, as they selectively absorb radioactive iodine. External Beam Radiation: Employed for aggressive, recurrent, or inoperable thyroid cancer, this treatment uses high-energy X-rays to target and destroy cancer cells. Thyroid Hormone Replacement: Following a total thyroidectomy, levothyroxine medication is prescribed to replace the hormones typically produced by the thyroid. Chemotherapy: Reserved for advanced or aggressive cases, chemotherapy is not the first-line treatment for thyroid cancer. Prevention and Risk Reduction: Iodine Intake: Maintaining a diet with adequate but not excessive iodine is vital for overall thyroid health. Most developed countries offer iodized salt to prevent iodine deficiency. Limit Radiation Exposure: Reducing exposure to ionizing radiation, especially during medical procedures, is essential. Discuss potential risks and benefits with healthcare providers. Regular Check-ups: Regular visits to healthcare providers for thyroid examinations are crucial, particularly with a family history of thyroid cancer. Early detection is key to better outcomes. Conclusion: Thyroid cancer encompasses various types and presentations. Early detection and appropriate treatment are pivotal for optimal outcomes. If you have concerns about thyroid health or experience symptoms, consult a healthcare professional for a comprehensive evaluation and personalized guidance.
Salivary gland tumors
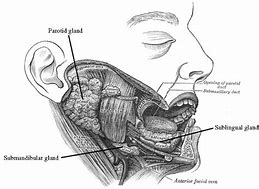
Salivary glands are responsible for producing and secreting saliva, which plays a crucial role in digestion, lubricating the mouth, and maintaining oral health. One of the three primary salivary glands in the human body is the Parotid gland. The parotid gland is the largest of these salivary glands and is located near the ear, extending down to the jawline on both sides of the face. Parotid cancer, also known as parotid gland cancer, is a relatively rare form of cancer that originates in the parotid gland. Parotid cancer can be challenging due to its location and the complex facial structures surrounding the parotid gland. TYPES OF PAROTID CANCER Parotid cancer can encompass several histological subtypes, each with unique characteristics: Mucoepidermoid Carcinoma: This is the most common type of parotid cancer. It consists of a mixture of muco-secreting cells and epidermoid (squamous) cells. Tumors may vary in aggressiveness. Adenoid Cystic Carcinoma: Known for its slow growth, adenoid cystic carcinoma can be locally aggressive, and it tends to invade nerves, making complete surgical removal challenging. Acinic Cell Carcinoma: Acinic cell carcinoma is characterized by cells that resemble serous acinar cells. It often has a more favorable prognosis compared to some other subtypes. Salivary Duct Carcinoma: Salivary duct carcinoma is a high-grade malignancy often associated with facial nerve involvement. It tends to be aggressive and may spread rapidly. Adenocarcinoma: Adenocarcinomas are a group of cancers originating in glandular cells. Their behavior and aggressiveness can vary. Causes and Risk Factors: The exact causes of parotid cancer are not well understood. However, there are some risk factors that have been associated with an increased likelihood of developing parotid cancer. These risk factors may include: Exposure to ionizing radiation, such as previous radiation therapy to the head or neck. A family history of salivary gland tumors or a personal history of salivary gland tumors. Certain genetic conditions, like Cowden syndrome or familial adenomatous polyposis (FAP), which can raise the risk of parotid cancer. Symptoms: Parotid cancer may present with a variety of symptoms, including: A Painless Lump or Swelling: Most often near the ear or jaw area, which is the most common initial sign. Facial Weakness or Paralysis: Especially if the cancer affects the facial nerve. Difficulty Opening the Mouth due to tumor growth. Persistent Pain in the parotid area. Numbness or Weakness: It happens usually on one side of the face. Difficulty Swallowing: As the tumor grows, it can cause swallowing difficulties, potentially resulting in choking or discomfort. Diagnosis: Diagnosing parotid cancer involves a series of steps, including: Physical Examination: A healthcare provider will examine the affected area for any lumps or other abnormalities. Imaging Studies: These may include CT (computed tomography) or MRI (magnetic resonance imaging) scans to visualize the tumor and assess its size and location. Biopsy: A fine-needle aspiration (FNA) biopsy is often performed to obtain a tissue sample from the tumor for examination. In some cases, a surgical biopsy may be necessary for confirmation. Treatment: The treatment for parotid cancer is highly individualized and depends on factors such as the stage of the cancer, the specific histological subtype, and the patient’s overall health. Treatment options may include: Surgery: Surgical removal of the tumor, part of the parotid gland, or the entire gland is a common treatment. The extent of surgery depends on the stage and location of the cancer. Radiation Therapy: Radiation therapy may be used after surgery (adjuvant therapy) to eliminate any remaining cancer cells. It can also be a primary treatment for inoperable tumors. Chemotherapy: While not typically the primary treatment for parotid cancer, chemotherapy may be considered in cases where the cancer has metastasized (spread to other parts of the body). Targeted Therapy: In some cases, specific subtypes of parotid cancer may respond to targeted therapies that interfere with the mechanisms driving cancer growth. Prognosis: The prognosis for parotid cancer varies significantly based on several factors, including the stage of the cancer, histological subtype, and the effectiveness of the chosen treatment. Early detection and prompt treatment offer the best chances for successful outcomes, including a good quality of life after treatment. Patients diagnosed with parotid cancer are encouraged to work closely with their healthcare team to determine the most appropriate treatment plan and address their unique medical and personal needs
My Publications